[Killer Covid Protocols] Documentary “On A Knife’s Edge”
- Updated:1 year ago
- Reading Time:47Minutes
- Post Words:12402Words
Hoodie and John screen an incredible documentary on the notorious Hospital Protocols in Victoria, “On a Knife’s Edge”, which was created by the wife of Judah, to warn others about the Covid-19 protocols and to share their story of how her husband ended up on a ventilator, was given Remdesivir and end-of-life drugs including Midazolam & Fentanyl, acquired ventilator associated pneumonia, and almost died too many times to count from their ‘treatments’.
She methodically states the dates, facts, studies, and what was known at the time these protocols were given, and the heartbreak of not being allowed into the hospital as days turned into weeks, and weeks turned into months.
March 28, 2023 Rumble | Telegram
Pre-Documentary screening chat between Hoodie (ex Qantas pilot) and John Larter (former Paramedic)
Australia is in the middle of a health crisis. There is a lack of confidence in the health system. The health system has been duped. The health system has been corrupted. We’re hearing stories time and time again of people who have been severely vax-injured, who go to doctors and are pressuring employees to record these vaccination injuries. They’re only being told by doctors that they’re suffering from anxiety and just to go home and get over yourself.
We’ve got doctors who have admitted to us privately and to other doctors that the reason they’re not recording these and they’re not speaking up is because they’re scared they’ll be deregistered and they’ll lose their income.
Look, people have just lost complete faith in the health system in this country and for good reason. We’ve been lied to. We’ve been manipulated. There’s been coercion. There has been censorship.
There is no science in this job because you can’t have science when there’s censorship, and voices of reason are being squashed out.
This documentary is really going to open some eyes and we just hope and pray that we can do some good with this one.
As we bring forward another major exposé after the coming coming episodes discussing with a doctor who will be remaining anonymous because he’s actually working to save the vaccine injured and and if he speaks out now and is known, they’ll shut him down.
The lies, the betrayal of patient trust, the complete disregard for families, the story that unfolds here hoodie, it’s absolutely disgraceful, and how AHPRA is not chasing after these doctors and health care professionals that have just set aside their oath.
They have not carried themselves with dignity through this. In fact, if they think they are doing themselves a service by staying afloat during this COVID mess. I tell you now, they are going to need a life jacket that is unbelievable in proportion to what’s been seen now. Nobody will go to a doctor or one of these doctors that has peddled this nonsense for the past two years and covered it up. They won’t be able to get anyone through their door.
Yeah, that’s true, and, we talk about massive health budgets in this country. But John, it doesn’t translate to people’s lives being saved. We’re seeing health bureaucracies getting bigger with the funding that’s being expended on the hospital system and the health system. It’s not equating the beds and nurses and doctors, and we are in a severe crisis. Now, it’s clear, that there is there is gross deception in this whole debacle about health. There is corruption. There is incompetence. There’s ineptitude, and something has to be done to bring this to bring this to a halt and get this restored and get it back on its feet.
People have just completely lost confidence in health and this documentary shows exactly why. So thank you all for watching. We hope you enjoy this documentary and we’ll come back to you when you finish watching it. Thank you and see you shortly.
Documentary: On A Knife’s Edge
Called the ambulance
The World Health Organisation has declared coronavirus a global pandemic. There’s confirmation the coronavirus has reached Australia. Victoria will be in lockdown.
At the end of 2021, my life began to spiral downhill at a rapid rate. My husband and I had been sick for two weeks, but at around 1 a.m. on December 17th, 2021, my husband became dehydrated and delirious after not drinking for three days. So I made the fateful decision to call the ambulance.
At 2.28 a.m., the paramedics arrived and recorded that there was, “no immediate life threat”.
Ambulance records indicate that at 2.40 a.m., they gave my husband oxygen therapy while at the scene. However, I was there with him and he was not given any oxygen therapy the entire time while he was at home. The paramedics did, however, put a disposable protective face mask on him and asked me to do the same. He did not have any problems with his breathing at this stage.
Due to the government’s harsh COVID-19 restrictions at the time, the paramedics wouldn’t allow me to go with my husband, nor would they let me go into the hospital to be with him.
I was extremely concerned at this stage because I’d heard many horrible stories about unvaccinated people being wrongly treated due to bad hospital protocols and having horrific, often fatal, outcomes.
The very first thing the hospital did, without getting his consent, was test him for COVID using a PCR test, which returned a positive result. However, PCR tests had already been known to be unreliable.
- ABC News published an article on 4 June 2021 after two of Melbourne’s COVID-19 cases had been found to be false positives. (01) Two of Melbourne’s COVID-19 cases have been found to be false positives — how does that happen? https://www.abc.net.au/news/2021-06-04/covid-victoria-false-positive-cases-test/100190076
- Dean Whiting, a trained clinical biochemist and CEO of Pathology Technology Australia said, “false positives and false negatives are inevitable. They do happen and they will continue to happen”.
- The Therapeutic Goods Administration, TGA, is Australia’s government authority who monitor, regulate and make determinations on therapeutic goods such as drugs and medical devices. The TGA have admitted that the PCR test cannot distinguish between a live virus and a dead virus. (02)2022 MAY 14 TGA have finally admitted that the PCR test doesn’t distinguish between a live and dead virus. ~ Senator Gerard Rennick … Click for full citation
However, once they had confirmation of a positive PCR test, they placed him in an isolated area, put him on oxygen, a high flow nasal cannula, and would not allow any visitors, even vaccinated ones.
Hospital staff also warned him on his first day of being admitted that he may have to be intubated, to which he said he did not want that, and they replied, so you are requesting Do Not Revive?
He was shocked by their response and informed them that he wanted to try other options first, which they said they would do.
I spoke to him later that day and he was back to his normal self again after being rehydrated, besides suffering from common cold flu symptoms.
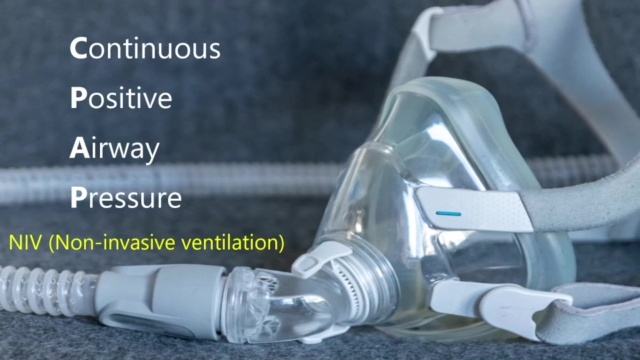
He wasn’t having any difficulty breathing, however the hospital kept him bedridden, and at 8.58 am, they decided to remove the high flow nasal cannula and place him on a more intensive oxygen therapy, called a BIPAP machine.
BIPAP stands for Bilevel Positive Airway Pressure, which pushes air into the recipient’s strongest when the person breathes in. This oxygen therapy is classed as a non-invasive ventilator.
The National COVID-19 Clinical Evidence Task Force provides a conditional recommendation for use of Remdesivir in adults. In August 2021, their guidelines stated, “Do not start Remdesivir in adults hospitalized with COVID-19 who require ventilation”. Down further, it clarifies that this includes both invasive and non-invasive ventilation. (03) National Covid-19 Clinical Evidence Task Force – Caring for people with COVID-19 https://clinicalevidence.net.au/covid-19/ (04) Australian guidelines for clinical care of people with COVID-19 – ‘Do not start remdesivir in adults hospitalised with COVID-19 who require non-invasive or invasive ventilation.” https://app.magicapp.org/#/guideline/7139/rec/142950

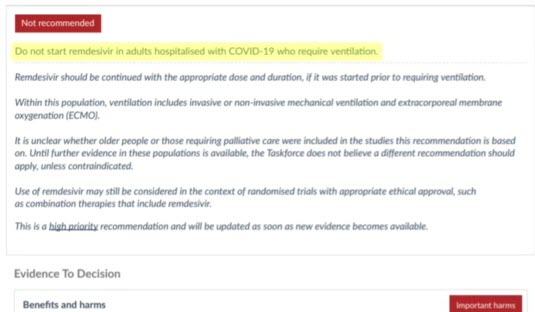

My husband had been on a non-invasive ventilator for over 3 hours, then at 12.15 pm, the doctors went against the National COVID-19 Clinical Evidence Task Force recommendation and administered the first dose of Remdesivir to him. (05) All Things Remdesivir https://pennybutler.com/remdesivir/
They did not inform him of any potential risks associated with this drug, and they did not inform me they were beginning this treatment. I only found out he was being given remdesivir five days later when I asked what medications were being administered to him. (06) Don’t use Gilead’s remdesivir in hospitalised COVID-19 patients, WHO says – November 2020 – https://www.reuters.com/article/us-health-coronavirus-remdesivir-who-idUSKBN28000Q
At 12.26 pm, the hospital switched from the BIPAP machine to a CPAP, which is also classed as a non-invasive ventilator. CPAP stands for Continuous Positive Airway Pressure. However, this one forces constant bursts of air into his lungs at an uncomfortably high and fast rate. He was not informed of any potential risks from using this device. Neither was he asked if he would like to begin this treatment.
At the time, the CPAP machine was a fairly new treatment being used for COVID patients. However, new studies are finding that these machines are not only ineffective, but they can be dangerous. Due to COVID-19 being a new virus, the effectiveness of a CPAP machine on a patient who is suffering with the illness wasn’t fully known.
However, what was established is that CPAP machines have been known to cause asthma, coughing, hiccups, difficulty breathing, reactive airway disease, pneumonitis and pneumonia.
CPAP Victoria’s website admits that, “the warm and humid environment of the heated tubing is perfect for fungal, mold and yeast growth. Hazardous organisms in the CPAP machine tubing could be blown directly to the user’s lungs. This could lead to airway and lung irritation, which may subsequently develop to pneumonitis, bronchitis and pneumonia.”
A study published in the Canadian Medical Association Journal examined the incidence of pneumonia in more than 34,000 patients who were divided into two groups, the CPAP users and the control group. Researchers found that CPAP users were 32% more likely to develop pneumonia compared to the control group. In general, a weakened immune defense can make a patient more vulnerable to different types of lung infections. It’s important to note that this study was only observed on patients using the CPAP machine overnight, not on a continual 24-7 basis like my husband received. (07)Su VY, Liu CJ, Wang HK, Wu LA, Chang SC, Perng DW, Su WJ, Chen YM, Lin EY, Chen TJ, Chou KT. Sleep apnea and risk of pneumonia: a nationwide population-based study. CMAJ. 2014 Apr 1;186(6):415-21. doi: 10.1503/cmaj.131547. Epub 2014 Mar 3. Erratum … Click for full citation
The Lancet is the world-leading source of clinical, public health and global health knowledge, ranking first among all general and internal medicine journals globally. Regarding the use of CPAP machines as treatment for COVID-19, they published the following. “In summary, this study shows no evidence of a survival advantage from CPAP treatment as a ceiling of care in severe COVID-19 pneumonitis when compared to conventional oxygen therapy. CPAP administration in the ward setting has high mortality and may bring a significant treatment burden to patients”. (08)Bradley P, Wilson J, Taylor R, Nixon J, Redfern J, Whittemore P, Gaddah M, Kavuri K, Haley A, Denny P, Withers C, Robey RC, Logue C, Dahanayake N, Min DSH, Coles J, Deshmukh MS, Ritchie S, Malik M, Abdelaal H, Sivabalah K, Hartshorne MD, Gopikrishna … Click for full citation
Another study that was done on COVID-19 patients undergoing CPAP therapy showed grim results. “A retrospective study reported failure rates of 66% in patients with COVID-19 receiving CPAP and high mortality 55% in those requiring invasive mechanical ventilation after CPAP failure.” (09)Gorman E, Connolly B, Couper K, Perkins GD, McAuley DF. Non-invasive respiratory support strategies in COVID-19. Lancet Respir Med. 2021 Jun;9(6):553-556. doi: 10.1016/S2213-2600(21)00168-5. Epub 2021 Apr 16. PMID: 33872588; PMCID: PMC8051928. … Click for full citation (10)Radovanovic D, Coppola S, Franceschi E, Gervasoni F, Duscio E, Chiumello DA, Santus P. Mortality and clinical outcomes in patients with COVID-19 pneumonia treated with non-invasive respiratory support: A rapid review. J Crit Care. 2021 Oct;65:1-8. … Click for full citation
The doctors said the X-rays look bad and put him on antibiotics and his first round of Covid Antivirals, which included Baricitinib, and a ten-day course of Remdesivir.
Towards the end of 2020, the New York Times published an article that stated, “Remdesivir, the only antiviral drug authorized for treatment of COVID-19 in the United States, fails to prevent deaths among patients according to a study of more than 11,000 people in 30 countries sponsored by the World Health Organization”. (11) Remdesivir Fails to Prevent Covid-19 Deaths in Huge Trial https://www.nytimes.com/2020/10/15/health/coronavirus-remdesivir-who.html
Not only was this drug shown to be ineffective, it also has been proven to be dangerous and is known for causing kidney failure. This was published on the National Institutes of Health website. (12)Silva NAO, Zara ALSA, Figueras A, Melo DO. Potential kidney damage associated with the use of remdesivir for COVID-19: analysis of a pharmacovigilance database. Cad Saude Publica. 2021 Nov 12;37(10):e00077721. doi: 10.1590/0102-311X00077721. PMID: … Click for full citation
An earlier study had been done in 2019 on Remdesivir to see how effective it was at treating Ebola. The result showed, “the mortality rate in the Remdesivir treatment group 53%”. (13) Investigational Drugs Reduce Risk of Death from Ebola Virus Disease https://www.nih.gov/news-events/news-releases/investigational-drugs-reduce-risk-death-ebola-virus-disease
A registered nurse for over a decade and founder of American Frontline Nurses, Nicole Sirotek worked at a hospital in New York at the beginning of the COVID-19 outbreak. She did not see any patients die from COVID-19, however many patients were dying.
Rumble | Telegram | Full Testimony
“I didn’t see a single patient die of COVID. I’ve seen a substantial number of patients die of negligence and medical malfeasance.”
“Now, when I was there and I saw that the pharmaceutical companies were rolling out Remdesivir onto the patients, I tried to get a hold of the IRBs, I tried to get a hold of my appropriate chain of command, I tried CMS, I tried Department of Health, and they rolled out Remdesivir onto a substantial number of patients for which we all saw it was killing the patients, and now it’s the FDA approved drug that is continuing to kill patients in the United States.”
“As nurses, we’ve collected a statistical or descriptive amount of information that you may not get from the doctors because for more they do quantitative data. We do qualitative data with a humanistic phenomenological approach in nursing research, and so we’ve collected the data from all of these patients across the country, all of these data pool shows that as these patients get Remdesivir, they have a less than 25% chance of survival if they get more than two doses.”
My husband was moved from the emergency department to the ICU and was told by our doctors that “COVID has caused him to have acute kidney failure”. Not attributing it to the fact that he was severely dehydrated. They also told him that “due to COVID”, he now has a permanent heart condition.
By the end of his first day in hospital, he was already on a strong concoction of medications with most of their side effects warning of the potential to cause serious health problems, especially difficulty breathing.
Thankfully, the next day I received a call from a doctor who told me that his kidney issue had been all sorted and is now back to normal and that he never had a heart condition.
I had heard that Ivermectin was an alternative treatment that has been found to be effective in treating patients with COVID, so I asked the doctor if they could give him Ivermectin. The doctor laughed, then proceeded to tell me that it’s not proven to help and isn’t part of their “protocols”.
The doctor wrote in my husband’s medical report, “raised question of Ivermectin – advised it is not part of our guidelines/protocols and he is receiving other COVID therapies, baracitinib / remdesivir / dexamethasone”.
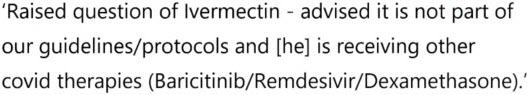
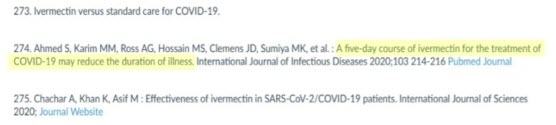
Interestingly, two clinical trials noted in the references section of the Australian guidelines for the clinical care of people with COVID-19 show evidence that Ivermectin is effective in reducing the duration of the SARS-CoV-2 virus.

In the guidelines it says, “a five day course of Ivermectin for the treatment of COVID-19 may reduce the duration of illness”. This was published in the International Journal of Infectious Diseases on 2nd December 2020.
The other statement says, “favorable outcome on viral load and culture viability using Ivermectin”. This was first published in Med Archive on 31st May 2021.

The guidelines also include a pilot trial that was studied in 2021, with results showing that Ivermectin caused a 5,000 fold reduction in viral RNA that all patients got over the virus faster with the use of Ivermectin and that this drug did not cause any serious adverse events. The article has since been retracted.
These articles were published well before my husband became sick with the virus.
For the next five days, my husband was kept on the CPAP machine day and night, with only minimal time offered to eat, drink and change over to the high flow nasal cannula for short periods.
Throughout this timeframe, on December 21st, the doctor informed me that my husband has bacterial pneumonia, to which he said they’re giving him a 7-day course of antibiotics for. There was no mention of pneumonia until this date.
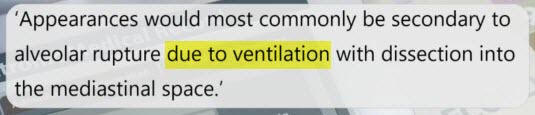
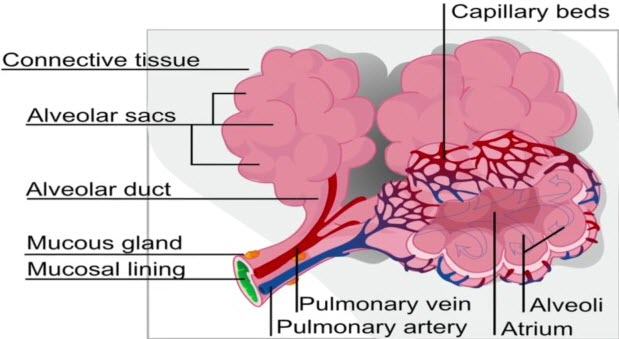
The report from the radiology registrar revealed a different story from what I’d been told by the doctor. The report stated, “appearances would most commonly be secondary to alveolar rupture due to ventilation with dissection into the mediastinal space”. Alveoli are organized into clusters and each cluster is grouped in alveolar sacs. Alveoli are tiny air sacs in the lungs that exchange oxygen and carbon dioxide during the process of breathing in and breathing out.
Damage to the alveoli and airways makes it harder to exchange carbon dioxide and oxygen during each breath. This report concludes that the ventilator has caused damage to my husband’s lungs. The radiologist also noted that my husband had new Subcutaneous emphysema and Pneumomediastinum.
He was additionally diagnosed with Barotrauma and Pneumonitis. None of these details were divulged to my husband or me.
I asked the doctor about whether they could give him vitamin D and vitamin C, natural supplements that have been proven to help recover from COVID. However, he said there’s no evidence that it’s useful for COVID.
He wrote in the medical report:
I spoke to the dietitian and asked her if they could put my husband on vitamin C and vitamin D, but the dietitian said they can only give those supplements if the patient is low on them.
She wrote in the medical report, “advised we do not routinely prescribe this. We could check levels and replace if it is low, but not without a clinical need to.” “Wife appears to be requesting for covid purposes.’

In 2020, studies showed that the use of vitamin C and vitamin D can help reduce the severity of COVID-19. (14) Politics Block Lifesaving Medicines To COVID Patients https://pennybutler.com/blocking-lifesaving-meds/ (15) Stuck In A COVID Ward? https://pennybutler.com/covid-ward/ (16) Viral Replication (How To Reduce Viral Load & Prevent Worsening Disease) https://pennybutler.com/viral-replication/ (17) Ways To Protect Yourself If You Haven’t Had The Jab (Or Even If You Have) https://pennybutler.com/part5-sars-cov-2/
On December 22nd, I asked if they were treating him for asthma, something he’s had to have daily medication for his whole life. However, the doctor said they are not. They also did an ultrasound on his lungs for any potential blood clots, and it came back all clear and showed his heart function was perfectly normal.
My husband was starting to feel out of breath for the first time on this day, something he hadn’t felt until now after being on the CPAP machine for five days and nights.
Another important note is that my husband got out of bed on this day and sat in a chair, the first time since being admitted to hospital. He had been lying flat on his back in bed for five days straight, creating the potential for yet another prospective disaster resulting in pneumonia.
WebMD.com states, lying flat on your back for a long time can increase your risk of developing pneumonia.
By the 23rd of December 2021, my husband was at the point where he believed what the doctors and nurses had been telling him throughout the past week, that he couldn’t survive without the assistance of the oxygen. What was confusing to him though, was that he felt he could breathe better without the oxygen mask than with it. The doctors said to him that this is the only way he’s going to get better.
They also told him he had now developed pneumonia, something he hadn’t been told until this day. He wasn’t given any more information than that, so he had no idea what sort of pneumonia it was or how he had developed it.
The medical report sheds more light as to what type of pneumonia he had developed. The report states three letters, V-A-P, which is the abbreviation for Ventilator-Associated pneumonia. Ventilator-associated pneumonia is a lung infection that develops in someone who’s on a ventilator.
My suspicions were confirmed that the continual use of non-invasive ventilation with the CPAP caused him to acquire pneumonia. Both the radiologist and the doctors separately confirmed that their ventilation policy has been the cause of my husband developing this pneumonia.
Another problem that was written on his record this day was superimposed H-A-P, which is hospital-acquired pneumonia. This information was never given to me or my husband, so we were completely unaware of this at the time.
Hearing he had pneumonia was frightening and overwhelming for him. He started to become more weary of the treatment he was being given and told me he wanted to go home tomorrow morning, so we started making arrangements.
We planned that I would call the hospital first thing the next morning, informed them that he would like to discharge himself and that I would go and pick him up.
On December 24th, 2021, exactly one week after being administered to hospital, I packed his bags and was ready to go and get him, but at 9.30am the doctor called to tell me that they need to intubate him now, within the next ten minutes, stating that it’s dangerous not to. He said it’s safer to intubate him now while it’s not an emergency and while they have the anesthesiologists there ready to go, rather than wait and have to do it later when they don’t have the anesthesiologists on hand.
I felt shock and dread come over me because this was the very thing I was fearful of happening. I asked if I could come in and see him before they put him in an induced coma or at least speak with him on the phone before they do the procedure, but the doctor flatly denied both my requests, repeating that, “it’s too dangerous to wait”, and that they have to do it now.
I asked if my husband had agreed to being intubated to which the doctor replied, “I’m not asking for your permission, I’m just telling you what we’re going to do whether you agree or not.”
I was taken back by his court response as well as the fact that he didn’t even address my question, so I explained that I knew he wasn’t asking for my permission, but that I wanted to know if my husband had agreed to be intubated to which the doctor replied, yes he has. He ended the conversation by telling me they will let me know once it’s been done.
The doctor wrote in the medical report, “Explained that this is not a routine courtesy call, rather it is regarding imminent intubation. At this time this is able to be done by the airway experts, an aesthetic consultant in a controlled manner, and this is our plan. Although this is not without risk, it is being done by the experts. Inquiry made repotential visit into ICU. Response, this will depend upon COVID status”.
I desperately tried to contact my husband on his phone, but it had run out of battery, so there was no way we were able to communicate with each other before he was put into an induced coma.
An article published in the National Library of Medicine on September 2020 admits that, “There is no direct evidence attesting to the benefit of intubation and IMV in critically ill COVID-19 patients. On the contrary, a report revealed that of 32 COVID-19 patients who received intubation and IMV support, 31 died”. (18)Luo M, Cao S, Wei L, Zhao X, Gao F, Li S, Meng L, Wang Y. Intubation, mortality, and risk factors in critically ill Covid-19 patients: A pilot study. J Clin Anesth. 2020 Dec;67:110039. doi: 10.1016/j.jclinane.2020.110039. Epub 2020 Sep 7. PMID: … Click for full citation
A short time later, I received a call from the doctor informing me that my husband had been successfully put on the ventilator and is now fully sedated. He went on to explain how bad my husband was before he was intubated.
“He was needing like 100% oxygen. The machines were all maxed out. Hopefully, we’re going to get this down to stay below around 50%, 40%. Around that stage, if they’re doing quite well, then we slowly wean down the sedation, the sleeping medication and let them wake up. Usually a couple days. “
My precious husband, who I’d been married to for the past 25 years, had been given treatments where he ended up having severe lung problems and was put into an induced coma the day before Christmas. The rest of this day, Christmas Eve, and also Christmas Day, felt like a blur. I waited with trepidation in the hope that he would be woken up after only a few days and everything would be fine. A few days passed, but there was no mention of waking him. Although the doctors were saying that he seemed to be doing well on the ventilator and the oxygen levels he was requiring were slowly getting better.
Dr Brian Ardis, chiropractor, medical researcher and CEO of Ardis Labs, began researching hospital practices for patients with COVID-19 when he saw his father-in-law die after being treated with the hospital protocols. (19) Dr Bryan Ardis With the most stunning truth about Covid Fauci & Remdesivir you could never imagine https://www.bitchute.com/video/IC2LQQpieYl6/
“Still to date, they are calling it pneumonia from corona. They’re going to use remdesivir. 31% of people treated with COVID-19 will have acute kidney failure. Their lungs will fill with fluid. Right now they’re adding dexamethasone, which has 4% reported kidney failure for all those who get it. So now you’re up to 35%.”
“If anyone listening to this has a loved one in a hospital and they have added to that protocol, a drug called vancomycin, which is an antibiotic, upwards of 10% of all of those individuals will experience even worse acute kidney failure. It will stop their heart pressure on their heart, make them go into a coma and make them unconscious and they will die. And they will say it was because of COVID-19. This is not true.”
On the 29th of December 2021, a few days after doctors finished the treatment of Remdesivir and Dexamethasone.
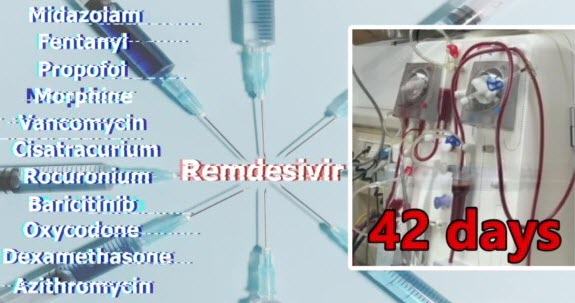
While my husband was still on Baricitinib, he was started on Vancomycin due to now acquiring sepsis. He was also on two sedation medications, Fentanyl and Midazolam. The medical report stated, “at risk of sudden deterioration given clinical status”.

On the 30th of December 2021, my husband was administered midazolam and morphine. Both of these drugs have separately been associated with respiratory distress. Midazolam and morphine together synergistically boost the respiratory depression effects of these drugs and the deadly toxic effects of the drugs.
“All of them make the respiration depression worse and you’re dealing with supposedly a respiratory distress syndrome and you’re going to add these sedation drugs as an excuse for ventilation on top of the toxic effects of remdesivir.” ~ Dr Bryan Ardis
My husband started out being sedated with only two drugs but after a short time, the doctors changed it to three sedatives, Propofol, morphine and midazolam. Every so often, morphine was swapped for Fentanyl or Oxycodone. He was also kept paralyzed a lot of the time as well, with doctors swapping between Cisatracurium and Rocuronium.
That same morning, the doctor called and I spoke with him at 9:16 a.m.
“He’s had a little bit of a wobble overnight and by that what I mean is that things have changed to the extent where for whatever reason he’s required more oxygen so that’s a bit of a concern. It’s not as comforting as the pictures was painted by my colleague yesterday. Wheels are not falling off at the moment, things are not drastically hitting downhill. It is a concern that things have actually changed in that sort of direction. Things are not quite the way we were hoping they were and have changed quite a bit. It’s a matter of quite serious.”
While I was still trying to process what I’d just been told, at 9:52 a.m. I received another call from the doctor. My heart sank because I knew that getting two phone calls from the ICU in the same hour was very serious.
The doctor informed me that because my husband had become so ill that they needed to put him on what’s called ECMO, a heart and lung machine. ECMO stands for extracorporeal membrane oxygenation and is classed as a last resort extreme form of life support. The ECMO machine takes over the job of the lungs to give them a chance to rest and heal. It pumps the blood out of the patient’s body, oxygenates it, then pumps it back into the body.
There are several ways ECMO can be set up. The doctors decided to place a cannula in both of my husband’s femoral veins. ECMO is the highest level of life support that can be provided, so if this didn’t work, there were no other options to help my husband survive. I was in complete shock. I felt like I’d hit rock bottom. I thought the ventilator was bad enough, but things just got a whole lot worse.
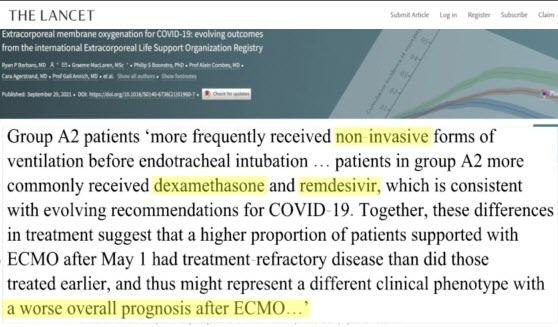
An international study published in the Lancet on October 2021 shows that there seems to be a decreased survival rate for patients who received the following treatments before being started on ECMO, non-invasive ventilation, remdesivir and dexamethasone. (20) Extracorporeal membrane oxygenation for COVID-19: evolving outcomes from the international Extracorporeal Life Support Organization Registry https://www.thelancet.com/article/S0140-6736(21)01960-7/fulltext
A doctor called again at 7:18pm to advise me that they found it very challenging to perform the procedure and that my husband’s oxygen levels went low for a prolonged period. Therefore, he may now have neurological damage. He pointed out that there’s no way of knowing for sure until it comes time to wake him up. Not only was I concerned that my husband may never wake up, adding to the concerns was that he may have permanent brain damage.
Something I wasn’t aware of was that the medical report noted that my husband now has MRSA, which is Methicillin-Resistant Staphylococcus aureus. This is a form of the superbug germ known as Staph or Golden Staph, which is a bacteria that is commonly found in hospitals and is resistant to several antibiotics.
My husband and I are Christians. We believe that the Bible is God’s written revelation to man, that all of mankind has sinned against God, but all who repent of their sins and place their trust in Jesus will be saved. I knew that God could heal my husband because I know that he is all powerful and he performs great miracles. My question wasn’t, could God heal my husband? It was, is it God’s will for my husband to live? I knew that if it was in God’s will for him to live, then God would bring him through.
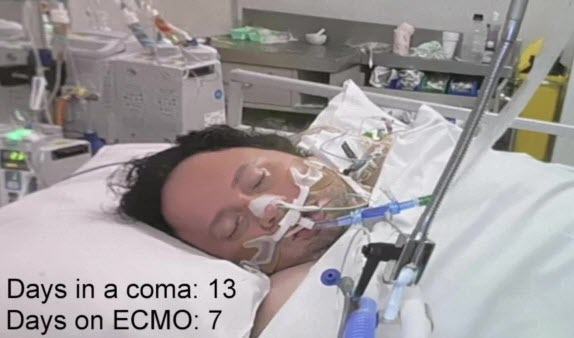
On 6th January 2022, at 10.59pm, 13 days after my husband was put into an induced coma, 7 days after being put on ECMO, the doctors contacted me to let me know that they are not happy with the amount of oxygen my husband is receiving with the current setup of the ECMO machine.
So they decided to do a procedure to reconfigure the ECMO and place a cannula into the jugular vein in his neck. I wasn’t informed of any problems that may have occurred while they were doing this procedure, however the medical records indicate that my husband’s oxygen levels went dangerously low during the process.
As the days passed, fear kept creeping in, with so much confusion, worry and questions rushing through my mind. How long will he be in a coma for? When will his lungs start working? Will he ever wake up? Hours turned into days. Days turned into weeks. Weeks turned into months.
During this entire period of time, not once was I allowed to enter the hospital to be with my husband. Even though the doctors continually emphasised the seriousness of the situation, the hospital would not let me come in because I was unvaccinated.
Going through such a horrifying ordeal with my husband’s life being on the brink of death was bad enough, but to be deliberately stopped from physically being with him was a whole other level of overwhelming grief.
With so much time passing, days felt like years and nights were filled with loneliness. My life partner, who I do everything with, was no longer with me. He was unknowingly fighting for his life. I feared that this moment of separation may become permanent. I couldn’t go into the hospital, I couldn’t sit with him and hold his hand.
But I could pray. I studied the scriptures and found instances where the Lord heard and answered the prayers of his people. I began to read these scriptures day and night, praying for my husband and clinging on tightly to my God. I told him all my doubts and fears, asking him to please intervene and save my husband from the grips of death. For the next two months I spent every waking hour praying, pleading and crying out to God, asking him to please heal my husband.
On the 15th of January 2022, my husband’s birthday, I received some very bad news. The doctor called at 6:39 p.m. and told me that my husband’s condition has worsened and that they’re very concerned about him. It started to sort of really, really struggle today, is showing signs of being at risk that it could get worse and we could then struggle to support him. It’s pretty concerning for us. We’ll see what happens in the next few hours.”
He also said that I should be prepared to expect a call in the middle of the night if things got worse. The doctor wrote in the notes, “seems to be deteriorating unfortunately”.
This was such hard news to hear, and on his birthday of all days. I went to bed that night hoping and praying that my phone wouldn’t ring.”
The next day on January the 16th, 2022, the doctor called at 6.38pm.
“He’s hanging in there, but he’s still hard going and we need everything to go right from here. We’re still very, very worried about him. If it looked like things were going to get any worse, we’d get you to come in.”
Due to my husband being in such a critical condition, I desperately pleaded with the hospital to give me permission to visit him. But the only reason they said they would allow me to go in to see my husband, was if he was at the point where he was going to die. Otherwise, we would continue to be kept isolated from one another.
On the 20th of January, 2022, my husband was diagnosed with pulmonary edema. This means he had too much fluid in his lungs. While the doctors were doing a circuit change for the ECMO, that is, changing the ECMO tubing, my husband’s oxygen saturation level went down to 37%.
The report states, “Nadia sets 37% with profound bradycardia plus ECG changes”. A normal oxygen saturation is between 95% to 100%. Anything under 80% can begin to affect the brain and is considered critical. Yet my husband’s oxygen saturation dropped to 37% on this day and 26% two weeks earlier.
I had moments where I felt like I was drowning, especially when a doctor called and delivered bad news. I received these types of calls almost every time a doctor made contact, and this kept happening for weeks on end.

Doctors said things like, he’s more unstable, he’s on a knife’s edge point, he’s very borderline. I had to keep bringing my mind back to God and reminding myself that I was not alone in this. I had to keep bringing my mind back to God and remind myself that he is ultimately in control of my husband’s life. I found that when I did this, I felt God’s peace, which I know was a peace that passes all understanding. Although whether my husband would survive this or not wasn’t certain, I was learning to lean on my God no matter what happens.
On the 23rd of January 2022, I spoke to a doctor at 3.15pm. He said that my husband is still very unwell, that his lungs still aren’t working properly and he’s requiring a lot of support from the ECMO machine. He said my husband may need to be on it still for weeks or even months.
Over the next several weeks, my husband had numerous complications such as many hospital acquired pneumonias, numerous infections, often sepsis, vasoplegia and fluid overload.
This last issue was the most problematic because they had to give him fluid and at the same time try to offload it with the dialysis machine. However, every time they started removing the fluid, this would interfere with the ECMO machine and cause it not to work sufficiently.
If the doctors were unable to run the ECMO machine effectively, then there was nothing else they could do for him. When my husband had too much fluid in his body, it was filling his lungs which could cause them more damage. Fluid overload can then put pressure on the heart and cause heart failure. As I found out another complication from the doctors each day or two, I continued to pray.
Little did I know at the time just how many issues my husband was suffering from, with many of them being life-threatening. Just dealing with one of those serious issues can be fatal. Yet my husband was enduring many at the same time.
On the 30th of January 2022, the doctor called at 10.20am to say that my husband aspirated the tube feeding formula, so he has some kind of bowel obstruction which may need life-saving surgery to fix it.
My family and I prayed and asked God to please clear whatever’s obstructing my husband’s bowel so he can receive the fluid through the feeding tube again. The doctors did a CT scan to see if they can find out what was obstructing the bowel, but there was no obvious sign of an issue.
The next day, on the 31st of January 2022, the doctors started feeding my husband through the feeding tube again, and this time he was able to absorb it. The doctors had no idea what had caused the obstruction, but the problem suddenly disappeared.
Each day that passed started to bring with it a glimmer of hope because my husband was still alive. Through the darkness of fear and pain, I began to see a ray of light, knowing that after everything that was happening to my husband, God was indeed holding him and keeping him alive. It’s amazing how when you have no control at all over what’s happening in your life, you realize just how little control you really have. How long we will live, or when we will die.
With my husband constantly being so close to death day in and day out, I felt like my life was falling apart. But it was in those moments that I knew God was there with me. I could get mad at God or blame him for being in this horrifying situation, but I knew that I had no right to blame him. Every breath I’m able to take is only available with thanks to the grace of God. The Bible is filled with believers suffering immense troubles, but through their tribulations we see how they responded to their situation, whether they had faith in God no matter what happened.
Sleep often evaded me and I had the ongoing concern that my phone would ring in the middle of the night with bad news. Although I failed to remain steadfast in faith every single moment, God was so gracious and he still inclined his ear.
On the 1st of February 2022, the doctors backed off the sedatives a little to see how my husband would react. During my video call with him, I could see him moving his head slightly and blinking every now and then. Just to see him move, even a little, was a wonderful moment for me. After seeing him on video calls lying in the hospital bed completely still for the last six weeks, it was another glimmer of hope to see him move, even a little.
On the 3rd of February 2022, 41 days in a coma, 35 days on ECMO, the doctor called at 6.56pm to tell me some news I’d been hoping and praying for since the start of this ordeal. He said my husband’s oxygenation has slightly improved and his lungs are finally starting to recover. This was the best news to hear.
After praying to God and asking him to heal my husband’s lungs for almost two months, with absolutely no change during that time, to finally hear this news was huge. I knew that God had heard my heartfelt prayers. I’d been brokenhearted and in the depths of despair, yet God never left me. Every few days my husband’s lungs continued to improve. Air on an x-ray looks dark, so when lungs are healthy, they will look dark on the image.
By the 12th of February 2022, they were well enough to work on their own. Over the next week, the doctors slowly reduced the amount of sedatives they were giving my husband to let him finally wake up.
On the 13th of February 2022, after being on ECMO for 45 days, the doctors were able to turn off the ECMO machine. My husband’s lungs were working on their own again.
On the 16th of February 2022, my husband was looking extremely distressed on the video call because of the breathing tubes he had down his throat. Less sedatives meant he was able to feel the tubes and it was extremely uncomfortable. Although he wasn’t fully aware of what was going on, they had reduced the sedatives enough so they could see how well he could comprehend instructions. Thankfully, God preserved my husband’s brain, even when his oxygen level got to its lowest of only 26 percent. He was able to appropriately respond to the doctors and was cleared of any neurological problems.
When he looked at me on the video call, I could see in his eyes that he knew who I was. I felt tremendous relief to see that my husband was not only almost fully awake physically, but that his mind was fully intact, just like the day I met him. This was another miraculous answer to prayer.
On the 18th of February 2022, after being sedated for 56 days, my husband was completely woken up. During my video call with him, he smiled for the first time since this whole nightmare began. It was such a moving moment. My daughter and I burst into tears. It was nice to finally cry happy tears.
However, our trials weren’t over yet. The doctor said my husband’s kidneys aren’t working, and he may have to stay on dialysis for the rest of his life.
On the 28th of February 2022, the doctors removed the tracheostomy tube from my husband’s neck. After being on a ventilator for 66 days, my husband was officially breathing on his own.
On the 2nd of March 2022, after spending 75 days in the ICU, the intensive care unit, my husband was finally moved into a ward. This was such exciting news because it meant he no longer had any life-threatening issues.
On the 4th of March 2022, the renal team informed my husband that because it’s been so long, because it’s been over five weeks since they’ve been waiting for his kidneys to kick in, they’re not expecting them to start working. They said his options were to either stay on dialysis indefinitely or have a kidney transplant. We spoke on the phone and I told him about how we saw God perform a miracle by healing his lungs.
So we continued to pray and ask God to please now heal his kidneys. 20 minutes later, my husband’s kidneys suddenly began working.
After being given many different drugs for two months straight, with each one having the potential to damage the kidneys, including remdesivir, as well as being completely reliant on dialysis for 42 days, his kidneys miraculously started up again.
Each day they continued to improve until they went back to functioning perfectly normal again.
My husband had to learn to move, talk, eat and walk again. He had lost all muscle mass and was severely deconditioned. So the simple movement of lifting a hand or an arm was something he couldn’t do. He was confined to a bed for many more months and had to build up strength over the course of a few weeks. He was confined to a bed for many more months and had to build up strength over time in order to move his body.
Over these last few months, I’d spent countless hours searching for a possible way that I could be allowed to go into the hospital to be with my husband, contacting their board, speaking with nurse managers, as well as the family liaison team. I let them know I was willing to take a rat test before entering and follow all their guidelines and asked that they’d allow me entry on compassionate grounds considering the seriousness of my husband’s situation. I even went to a GP and had a serology test done which showed that I have the COVID antibodies. However, it didn’t matter what I presented to them. Their answer was always the same. No vaccination, no entry.
I researched the government’s hospital visitation guidelines and found that according to the Victorian Minister for Health’s guidance for the pandemic order 2022, unvaccinated people are allowed to visit their loved one in hospital under two conditions. That they undertake and present a negative rapid antigen test on the day and wear an N95 face mask. So as a last-ditch attempt, I wrote another letter to the hospital detailing the government’s guidelines.
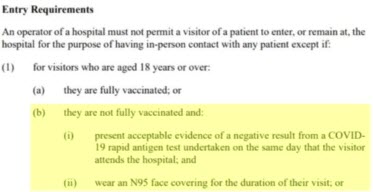
To my surprise, I received a call from the nurse manager in the ward informing me that they’re going to grant me permission to visit my husband.
On the 17th of March 2022, my husband was transferred to a rehab facility. He began sessions the following day to build up his muscles enough so he can walk again. Just when we thought all our problems were behind us, on the 3rd of April 2022, my husband began having immense pain in the right side of his stomach. The doctors did an ultrasound and found that he had cholecystitis, which is an inflamed gallbladder. He had to be rushed back to the hospital where they performed a cholecystostomy procedure, which is inserting a tube into his gallbladder in order to drain out the fluid buildup.
On the 20th of April 2022, my husband was transferred back to rehab where he was able to continue working at building up his muscles. So here he’s eating his lunch. Doing very good too, nearly finished. He’s quite enjoying that shepherd’s pie.
My husband’s medical report contains over 11,000 pages. His vaccination status was strewn throughout the entire document. The fact he was unvaccinated was mentioned at least 180 times.
While we’re thankful to the many doctors and nurses who helped my husband, the hospital’s protocols regarding how to treat an unvaccinated patient are proven to be extremely dangerous. Against all odds, my husband survived because God saved him.
Well, it’s been a long year to get to this part. I’ve gone through so much from December 17th, 2021, until now it’s been a tough journey. I’ve had to overcome a lot, I had to learn to walk again and feed myself and talk.
My voice still isn’t back to where it used to be because of the tubes that were down my throat and as well as the other things, the other procedures I’ve done, like a tracheostomy and things like that.
But I’m so blessed to be alive that I made it because so many people that went through what I went through didn’t and I find that a heartache.
Two people I know died while I was in a coma and they went through the same protocols that I went through which so many others went through and passed away. I think it’s a very sad thing that there’s been so much loss of life when it didn’t need to happen.
There was definitely rumours before I went to hospital that there were different protocols for those who were unvaccinated and those who were vaccinated and I can’t say whether that’s true or not in my case but what I can tell you is that the protocols that they followed were detrimental to my health including a cocktail of drugs and other medical equipment which was quite experimental for this type of issue that I had.
Quite honestly if I had left the hospital the next day after I had been rehydrated I don’t think I would have gone through the journey that I went through but they put so much fear into you to stay and the more you stay on these machines the worse your lungs get and it led me to a very bad place.
As you saw in this video I had 86 problems which I had to overcome, all kinds of problems and I’m really blessed that I’m not brain damaged or have any huge issues. I do have a little bit of memory loss. I can’t really walk that far yet. I can walk to the front of the house and back and things like that but I get very exhausted very quickly. Even having a shower is exhausting. So I’m praying for full recovery.
It’s been a miracle that I’ve come this far, that my kidneys healed when I was told that they wouldn’t heal, that I would need a transplant. When I prayed my kidneys came back 20 minutes after and this is after I had the terrible news that my kidneys would never heal and just through prayer, 20 minutes it all took for my kidneys to start working again.
I know that I’ve been very fortunate. It’s obviously not my time to go and I’m here for a reason. I really wouldn’t have got through this if it weren’t for my faith. I’ve been a Christian since I was 18 years old and I don’t know how people go through these things without God because I found it hard enough going through this with God. I know that He was comforting me and sustaining me all the way through. I really want to encourage you to seek the Lord because the days that we’re in right now are pretty tough and I don’t think it’s going to get any easier.
The world’s a bit of a crazy place and the agendas that are going on in government and on a worldwide scale, it’s very concerning.
With my own testimony when I was 18, I’d already grown up in a Catholic church but I didn’t really know God very well. God was somewhere in the distance for me. God was here and God was up in heaven and that was pretty much it. You just live your life the way that you want to and you never really think much of God. When I found out what Jesus had really done, that He died on the cross for me and that I would get forgiveness of sins because I found out that a holy God, that His standards are so high. I’ve been brought up to believe that as long as you’re not a murderer or a rapist, you’ll go to heaven. But then I found out that God’s law is so holy, that He’s so holy, His law, which reflects His holiness, is so high that even if you think a lustful thought, you won’t inherit the kingdom of God. You’ll end up in hell. I realized that I’d done so much more than thought of a lustful thought. I’d thought of all kinds of things, been angry at people and hurt other people, sinned against God, a holy God. I repented because I realized that I needed the Lord, I needed His forgiveness. I was filled with the Holy Spirit and since then I’ve never looked back.
Once I was filled with the Holy Spirit, I felt the presence of God every day. The depression that I felt at the time had gone. I had suicidal thoughts at the time that had gone. I’m not going to sit here and tell you that everything’s cured overnight when you become a Christian. It’s actually a hard life. It’s not always easy because we still have the flesh, we still have sin and temptation. It’s not an easy calling, but with the Holy Spirit there to guide you and lead you and for the Lord to comfort you, it’s possible. By His power only, not by anything that we do.
It’s about really becoming more and more like Jesus every single day. It’s only possible by His grace alone, not from our own efforts, but by His. I want to tell you this because I feel like it would be remiss of me for us to go through all this documentary for you to see the miracle that God’s done in my life.
One atheist doctor said to me that whilst I’ve never believed in God, she goes, after seeing your recovery, I do believe there must be a higher power.
Another doctor said to me that we call you the miracle man around here because they just never thought I would recover.
I think it would be remiss of me not to give you this good news. I just thank the Lord for everything He’s done, that He sustained my wife, my family through this heartache, through this hard time, and that He sustained me because without Him I don’t think I would have got through everything that was thrown at me.
It just seemed, when you look at everything, what I went through and what my body went through, it seems impossible that I would survive it. When you think about the 86 things that went wrong, when you think about just one of those things, let’s just pick one, kidney failure, or maybe let’s look at septicemia. I had that several times. You can have that once, sepsis, you can have that once and die from having sepsis alone. But that was just one of the 86 things. I had it many times. There were so many things that I survived. It’s just not possible for me to have survived what I’ve got through.
So I just thank you for watching, thank you for giving me this time and watching to this point. I know it’s not easy to hear a message like this. I never wanted to hear this kind of message when I was an unbeliever. I thought, yeah, yeah, yeah. But eventually, the seeds that people had planted in my heart, it took hold and it changed my life. So I’m just so grateful to have the support that I’ve had and my family and friends.
And I also, even though I do believe the protocols that they were in place, not just in Australia, but around the world, I do believe those protocols were terrible protocols.
I think there is massive agendas behind those protocols. It was agendas to drive up numbers with COVID, to make it look worse than it was. There was definitely agendas with the way that they used this equipment and the way that they gave these drugs.
But despite all that, despite the protocols, there are a lot of great nurses and doctors who do want to help and who are trying to care for people even through a bad situation. And I have many beautiful nurses that helped me that were so merciful and kind. So I thank them too.
My wife’s done a fantastic job with this documentary. It took so much time. She was sitting at the computer for 12 to 14 hours a day to get this done, to get this message out for you, to help you. I mean, I’ve gotten through this now, but I guess our concern is for other people and especially for the future, if they do this again, we want to warn you that you need to be very careful.
They say regarding COVID and the vaccine and things like this to weigh up the risks versus benefits. Well, I can tell you now, if I ever think of even going to hospital again, I’ll be weighing up the risks versus benefit of just going to hospital. I’m sorry to say that, but that’s just the way it is.
But if you have any questions, contact us. We love you. Thank you for watching. Take care and God bless. Bye-bye.
What did you make of that, John?
Well, that has to be almost one of the final flights of the dam busters. If that doesn’t crack the wall, Hoody, I don’t know what’s going to. It’s an absolute disgrace. It’s not only Victorian health that’s in crisis, but clearly I really appreciated what the Arlings said when they talked about, you know, there were good doctors and nurses in there supporting Judah as he was going through this ordeal. It’s clearly obvious, John, that the hospital protocols and policy is getting in the way of good health management. Yeah, look, the back of house of these organisations is out of control. There’s been a complete ignorance. There’s been a complete sellout. Falsehoods, lies, fraud, malfeasance. I mean, how do you sum it all up? I mean, it’s just too much to… It really is. I don’t know, Hoody. That has just left me gobsmacked, that video. That, to me, you know, is a journey through hell.
Yep. Stemming from what is basically a bit more than a common cold. There was no need to be hospitalised at all. It just seems, you know, it is out of control. So the upshot of this, John, is we will be interviewing the Arlings, Jen and Judah, in our next programme and we’ll discuss some of the aspects of the video and the drama that they went through. It’s absolutely outstanding and we trust you’ll all come back to watch our interview with the producer and the poor gentleman who went through this process in tomorrow night’s episode.
And I think once we’ve done that, Hoody, we’d have to almost follow that up with our expert panel to analyse both the documentary and the interview because, you know, what Philip Altman and others could reveal about the practices that went on in that hospital would be so… Oh, jeez, I don’t know. Horrifying.
Dear Lord, Father in heaven, we ask you to bless the Arlings, bless their family, Lord, and we thank you for their courage and we pray that this, as John said, will be a bomb that brings down the wall. Lord, as we go forward in seeking the truth, may you bring it to our attention so that this madness may end. We pray in Jesus’ name. Amen. Amen.
It’s often been heard to say… You just couldn’t make this stuff up. You couldn’t make this stuff up. Stay out of the trees, everyone. If you love somebody and you haven’t told them, please call them now and tell them. And we look forward to bringing you a wonderful interview with the family who brought you this documentary. Incredible stuff. God bless you and bye for now. Amen. Amen.
Graham & John talk with Jan and Judah about their experiences…
March 29, 2023 Rumble

Site Notifications/Chat:
- Telegram Post Updates @JourneyToABetterLife (channel)
- Telegram Chatroom @JourneyBetterLifeCHAT (say hi / share info)
- Gettr Post Updates @chesaus (like fakebook)
Videos:
References[+]
| 01 | Two of Melbourne’s COVID-19 cases have been found to be false positives — how does that happen? https://www.abc.net.au/news/2021-06-04/covid-victoria-false-positive-cases-test/100190076 |
|---|---|
| 02 | 2022 MAY 14 TGA have finally admitted that the PCR test doesn’t distinguish between a live and dead virus. ~ Senator Gerard Rennick https://telegra.ph/2022-MAY-14-TGA-have-finally-admitted-that-the-PCR-test-doesnt-distinguish-between-a-live-and-dead-virus–Senator-Gerard-Rennick-05-14 |
| 03 | National Covid-19 Clinical Evidence Task Force – Caring for people with COVID-19 https://clinicalevidence.net.au/covid-19/ |
| 04 | Australian guidelines for clinical care of people with COVID-19 – ‘Do not start remdesivir in adults hospitalised with COVID-19 who require non-invasive or invasive ventilation.” https://app.magicapp.org/#/guideline/7139/rec/142950 |
| 05 | All Things Remdesivir https://pennybutler.com/remdesivir/ |
| 06 | Don’t use Gilead’s remdesivir in hospitalised COVID-19 patients, WHO says – November 2020 – https://www.reuters.com/article/us-health-coronavirus-remdesivir-who-idUSKBN28000Q |
| 07 | Su VY, Liu CJ, Wang HK, Wu LA, Chang SC, Perng DW, Su WJ, Chen YM, Lin EY, Chen TJ, Chou KT. Sleep apnea and risk of pneumonia: a nationwide population-based study. CMAJ. 2014 Apr 1;186(6):415-21. doi: 10.1503/cmaj.131547. Epub 2014 Mar 3. Erratum in: CMAJ. 2014 Oct 7;186(14):1092. PMID: 24591276; PMCID: PMC3971026. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3971026/ |
| 08 | Bradley P, Wilson J, Taylor R, Nixon J, Redfern J, Whittemore P, Gaddah M, Kavuri K, Haley A, Denny P, Withers C, Robey RC, Logue C, Dahanayake N, Min DSH, Coles J, Deshmukh MS, Ritchie S, Malik M, Abdelaal H, Sivabalah K, Hartshorne MD, Gopikrishna D, Ashish A, Nuttall E, Bentley A, Bongers T, Gatheral T, Felton TW, Chaudhuri N, Pearmain L. Conventional oxygen therapy versus CPAP as a ceiling of care in ward-based patients with COVID-19: a multi-centre cohort evaluation. EClinicalMedicine. 2021 Oct;40:101122. doi: 10.1016/j.eclinm.2021.101122. Epub 2021 Sep 8. PMID: 34514360; PMCID: PMC8424135. https://www.thelancet.com/journals/eclinm/article/PIIS2589-5370(21)00402-8/fulltext |
| 09 | Gorman E, Connolly B, Couper K, Perkins GD, McAuley DF. Non-invasive respiratory support strategies in COVID-19. Lancet Respir Med. 2021 Jun;9(6):553-556. doi: 10.1016/S2213-2600(21)00168-5. Epub 2021 Apr 16. PMID: 33872588; PMCID: PMC8051928. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8051928/ |
| 10 | Radovanovic D, Coppola S, Franceschi E, Gervasoni F, Duscio E, Chiumello DA, Santus P. Mortality and clinical outcomes in patients with COVID-19 pneumonia treated with non-invasive respiratory support: A rapid review. J Crit Care. 2021 Oct;65:1-8. doi: 10.1016/j.jcrc.2021.05.007. Epub 2021 May 21. PMID: 34052780; PMCID: PMC8137355. https://pubmed.ncbi.nlm.nih.gov/34052780/ |
| 11 | Remdesivir Fails to Prevent Covid-19 Deaths in Huge Trial https://www.nytimes.com/2020/10/15/health/coronavirus-remdesivir-who.html |
| 12 | Silva NAO, Zara ALSA, Figueras A, Melo DO. Potential kidney damage associated with the use of remdesivir for COVID-19: analysis of a pharmacovigilance database. Cad Saude Publica. 2021 Nov 12;37(10):e00077721. doi: 10.1590/0102-311X00077721. PMID: 34787281. https://pubmed.ncbi.nlm.nih.gov/34787281/ |
| 13 | Investigational Drugs Reduce Risk of Death from Ebola Virus Disease https://www.nih.gov/news-events/news-releases/investigational-drugs-reduce-risk-death-ebola-virus-disease |
| 14 | Politics Block Lifesaving Medicines To COVID Patients https://pennybutler.com/blocking-lifesaving-meds/ |
| 15 | Stuck In A COVID Ward? https://pennybutler.com/covid-ward/ |
| 16 | Viral Replication (How To Reduce Viral Load & Prevent Worsening Disease) https://pennybutler.com/viral-replication/ |
| 17 | Ways To Protect Yourself If You Haven’t Had The Jab (Or Even If You Have) https://pennybutler.com/part5-sars-cov-2/ |
| 18 | Luo M, Cao S, Wei L, Zhao X, Gao F, Li S, Meng L, Wang Y. Intubation, mortality, and risk factors in critically ill Covid-19 patients: A pilot study. J Clin Anesth. 2020 Dec;67:110039. doi: 10.1016/j.jclinane.2020.110039. Epub 2020 Sep 7. PMID: 32920347; PMCID: PMC7476450. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7476450/ |
| 19 | Dr Bryan Ardis With the most stunning truth about Covid Fauci & Remdesivir you could never imagine https://www.bitchute.com/video/IC2LQQpieYl6/ |
| 20 | Extracorporeal membrane oxygenation for COVID-19: evolving outcomes from the international Extracorporeal Life Support Organization Registry https://www.thelancet.com/article/S0140-6736(21)01960-7/fulltext |
Truth-seeker, ever-questioning, ever-learning, ever-researching, ever delving further and deeper, ever trying to 'figure it out'. This site is a legacy of sorts, a place to collect thoughts, notes, book summaries, & random points of interests.
DISCLAIMER: The information on this website is not medical science or medical advice. I do not have any medical training aside from my own research and interest in this area. The information I publish is not intended to diagnose, treat, cure or prevent any disease, disorder, pain, injury, deformity, or physical or mental condition. I just report my own results, understanding & research.









































![[NWO] Bilderberg Group (Hollywood Actor investigates)](https://pennybutler.com/wp-content/uploads/2022/04/amrwaked-bilderberg.jpg)